West Coast medical FMs offer advice as COVID hospitalizations surge in other states
by Theresa Walsh Giarrusso
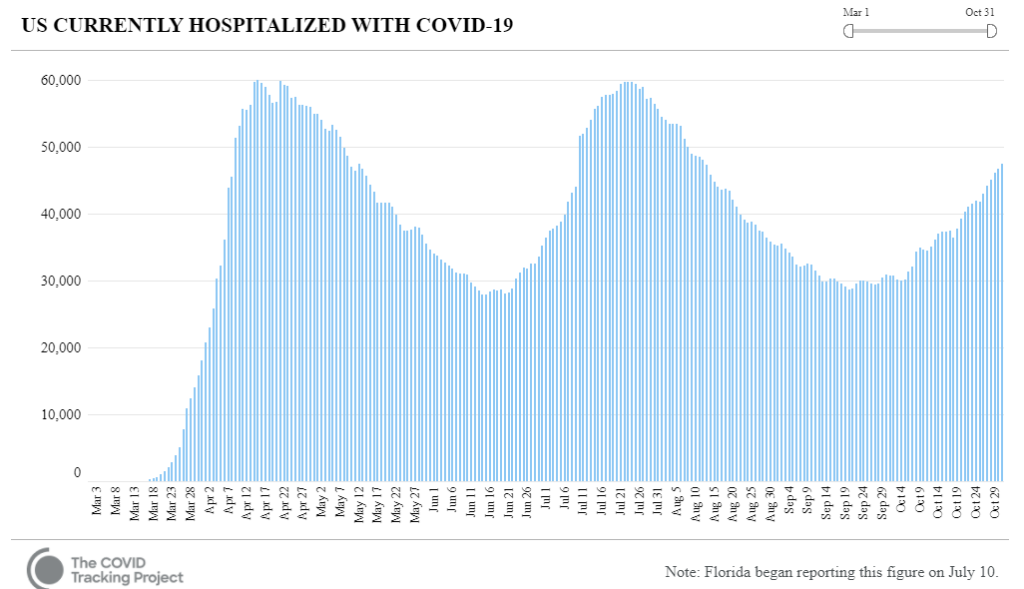
With U.S. COVID-19 hospitalizations jumping an estimated 46% by the end of October from the month prior, strained medical facilities are looking for strategies to meet the overwhelming demand on clinic space and staff. The situation is becoming critical in smaller, regional facilities with fewer resources than big cities and in states such as Idaho, Missouri, New Mexico and Utah, according to The New York Times.
West Coast medical facilities managers tangled with these same threats in the spring (and more with wildfires and smoke quickly following) and have much advice to offer their colleagues now. In September, 1 Hour Healthcare interviewed four of the top West Coast medical real estate executives to find out exactly what they faced and how they coped.
The episodes, “Recalibrating Medical Facilities Amid Disasters,” A Special 2-Part Report from California and Oregon,” are FREE for healthcare provider employees & AMFP members. Both parts of this episode are available now on-demand.
If you are not an AMFP member or healthcare provider employer, you can view each episode for $30. Click here for all the episodes.
The guests for these episodes were:
- Liz Brott, Principal Architect, Office Facility & Property Services, Sutter Health System.
- Ken King, Chief Administrative Services Officer, El Camino Hospital.
- Kerrie Bartel-Christensen, Executive Director-Oregon, Real Estate Strategy & Operations, Providence Health.
- Joel Swift, Director, Facilities Planning & Development, UC Davis Health.
The Interviewers were:
- Heather Chung, Vice President & Healthcare Studio Leader, SmithGroup.
- Jon Inman, Principal, Mazzetti, President, AMFP Northern California Chapter.
You will find a summary of strategies and best practices from all four conversations below, but you can click on each healthcare system’s name for more detailed excerpts. If you are a healthcare provider employee or AMFP member, you can watch the full episodes for FREE.
Heather Chung, Vice President & Healthcare Studio Leader, SmithGroup, and Jon Inman, Principal, Mazzetti, President, AMFP Northern California Chapter, conducted all four interviews and held a wrap-up discussion at the end of episode 5B. Here is a short summary of what they learned from all the guests and what big trends were mentioned.
Adaptability, flexibility and resiliency within facilities and staff were repeatedly stressed by our experts.
- The ability to make use of facilities within your health system and move patients and practices around depending on your needs.
- The ability to evacuate a facility, and maybe not shut it all the way down, so you can re-occupy easily and quickly.
- Outdoor space became indispensable. (See section below on all its uses.)
- Conversion-ready spaces and beds, where a room and bed may be deployed as med-surge, but then in the future or in a disaster response, it can be converted to an ICU capacity.
- The ability to create negative-pressure space whether its whole units or just individual rooms.
- The ability to control your airflow – 100% outside air for pandemic and then quickly switch to 10% when fires and smoke hit.
- Infrastructure flexibility for changing power, water, medical gas and data needs.
Flexible outside space became the star of the show and will be stressed in future planning.
- Our experts reported using outdoor space for many functions: pre-screening, triage, registration, clinical space, vaccination lines, pharmacotherapy checks, mother and baby checks and dropping off patients.
- The space needs to be flexible or have multiple areas where people could stay in their cars, where they felt safe, and be treated in care lines or for setting up treatment areas, such as tents.
- But you have to plan ahead for flexible outdoor space with utilities and infrastructure being built as you go or added to existing space.
- Outdoor space was also used as a staff respite when things got stressful.
Breaking down silos
- Integrating departments, such as Real Estate and Design and Construction with Facilities and Environmental Services, to create flexibility and strength. Kerrie Bartel-Christensen, Executive Director-Oregon, Real Estate Strategy & Operations, Providence Health, reported their integration was a tremendous organizational strength and allowed them to move in a coordinated fashion.
- Utilizing partners and cooperation outside of your health system for space, money for testing, use of closed facilities to benefit the community or state at large.
Trends for the future
- Pandemic pushed Telehealth forward. Our experts don’t think it’s going away. However, the jury is still out on how it will be applied: primary care, specialty care, mental health, PT? And where will it be conducted? Do you need rooms for this or do doctors work-from-home on those days?
- Make sure there are multiple points of entry to the facility and convertible space and interiors.
- Plan ahead for flexible outdoor space with utilities and infrastructure. (See above.)
- Infrastructure flexibility for power, water, medical gas.
- Make sure your IT infrastructure meets data usage needs and is secure from alternative locations and homes.
- Owning your clinics instead of leasing for more control over building exactly what you need for flexibility.
- Master planning alternative realities to make sure you have all the physical flexibility you need but also operational flexibility and a C-suite understanding of the options should disasters strike.
- Health systems investing in communities and providing good jobs for them.
