GP PRO responds to healthcare hand hygiene compliance data with tips for infection preventionists
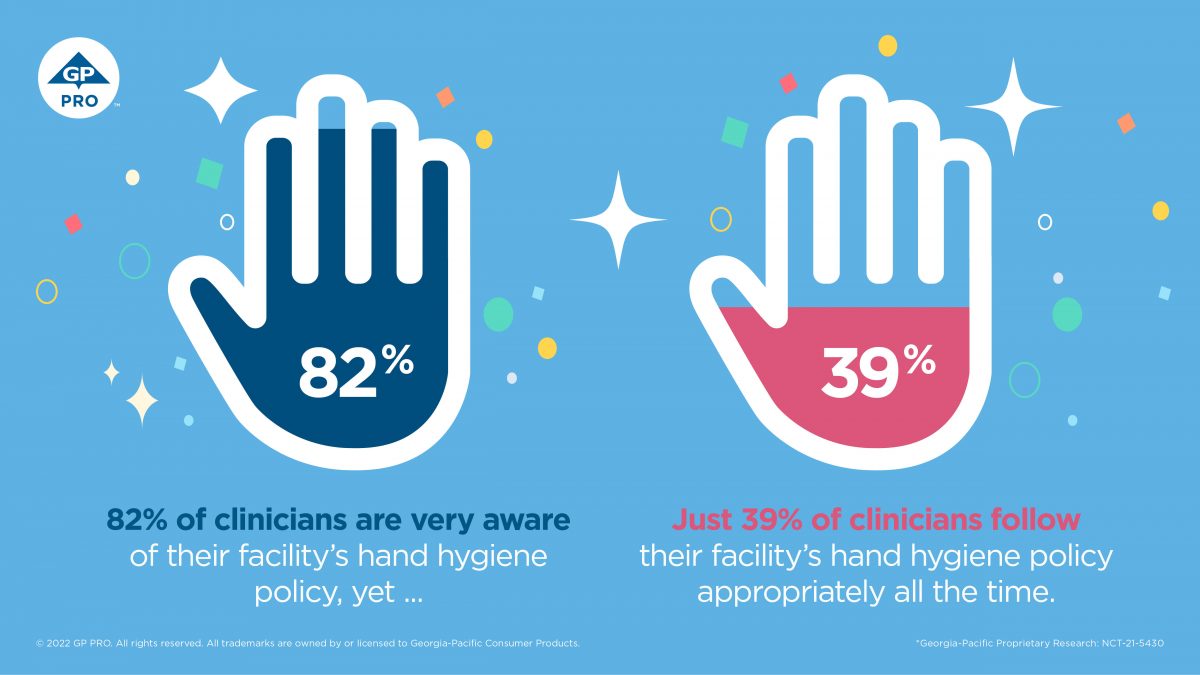
Graphic courtesy of GP PRO
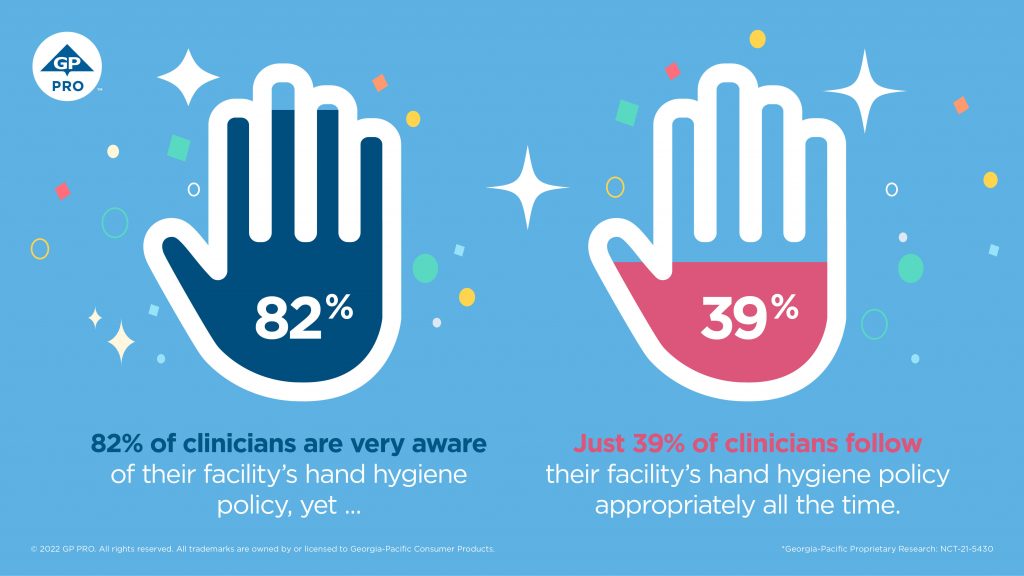
Earlier this year, GP PRO, a division of Georgia-Pacific helping to advance hygiene in healthcare and a wide range of other market segments, conducted proprietary research that found that just 39% of healthcare workers consistently comply with hand hygiene protocols primarily due to five common barriers. In response to those findings, GP PRO is releasing several recommendations to help infection preventionists influence and improve healthcare hand hygiene compliance.

According to the research (PDF file), conducted in November 2021, the five barriers healthcare workers face include 1) emergencies that require immediate attention; 2) a busy workload; 3) malfunctioning, broken or empty hand sanitizer dispensers; 4) full hands; and 5) difficulty during the glove-on / glove-off process — all of which are general inconveniences related to the nature of their jobs.
Healthcare workers often find themselves between a rock and a hard place. The very work they do combined with the physical location of sanitizer dispensers impedes their ability to quickly and easily sanitize their hands and comply with best practices. They simply should not have to choose between providing immediate emergency care and properly sanitizing their hands.
Ronnie Phillips, Ph.D., senior director of innovation with GP PRO’s Healthcare division
Phillips offers five recommendations for infection preventionists to consider as they strive to achieve sustained hand hygiene compliance among healthcare staff.
Seek input from clinicians
As GP PRO’s survey found, healthcare workers know when and why they are not complying with hand hygiene protocols. By gathering their input, infection preventionists have the knowledge and insight needed to develop an infection prevention program that is grounded in reality and set up for success. In addition, this staff perspective helps providers feel that they are part of the infection prevention solution and not just the problem.
Walk in clinicians’ footsteps
When it comes to mapping out the physical location of hand sanitizer dispensers, it’s important for infection preventionists to be aware of a clinician’s workflow as well as the patient’s continuum of care. Literally walking in a clinician’s footsteps clearly demonstrates how having a dispenser next to a patient’s bed allows for uninterrupted patient care versus having a dispenser near the entrance to a patient’s room.
Create transparency
Healthcare workers need to know exactly what metrics they are being monitored and measured against, how that monitoring and measurement is taking place, and that their peers are being monitored and measured in the same way. This kind of transparency drives believability in the hand hygiene program, which supports increased and sustained compliance, even when it’s inconvenient.
Properly maintain dispensers
Having well-placed but empty or broken dispensers is an easy way to create complacency with or disregard for hand hygiene protocols among healthcare workers. For this reason, any infection prevention program should include a maintenance plan. One suggestion is to leverage smart technology, such as GP PRO’s KOLO Smart Monitoring System, which alerts custodians when dispensers are running low or malfunctioning and helps provide healthcare workers with an assured, consistent supply.
Consider a wearable device
A wearable alcohol-based hand rub device that dispenses hand sanitizer and monitors hand hygiene activity puts healthcare workers in complete control of their hand hygiene. Such devices fit seamlessly into the clinical workflow and address several of the barriers to compliance clinicians provided in GP PRO’s survey. GP PRO’s SafeHaven Personal Hand Hygiene System combines a wearable, work-friendly sanitizing device with real-time, cloud-based reporting and personalized feedback. The always-present device delivers an alcohol hand rub anywhere, anytime, virtually eliminating common day-to-day hand hygiene disruptors.
Throughout healthcare, patience is necessary to achieve desired results, and hand hygiene is no different. Those recovering from surgery must be patient as their bodies heal. Those caring for the sick must be patient as medications take effect. When implementing these hand hygiene recommendations, infection preventionists must be patient as clinicians learn new behaviors, change their patterns, and make mistakes and learn from them. The good news is that change is possible!
Ronnie Phillips, Ph.D.
For more information, see the SafeHaven Infographic Insights Research Results (PDF file) on the GP PRO website.
